
Tuberculosis (TB) remains one of the most ancient and persistent scourges of humanity, a disease that has plagued us since antiquity and continues to pose significant health challenges worldwide. Despite the advent of modern medicine and substantial progress in our understanding and treatment of tuberculosis, it stubbornly remains a leading cause of illness and death, particularly in low- and middle-income countries. This article delves into the intricacies of tuberculosis, exploring its causes, transmission, symptoms, treatment, and the ongoing fight against this resilient disease.
What is Tuberculosis?
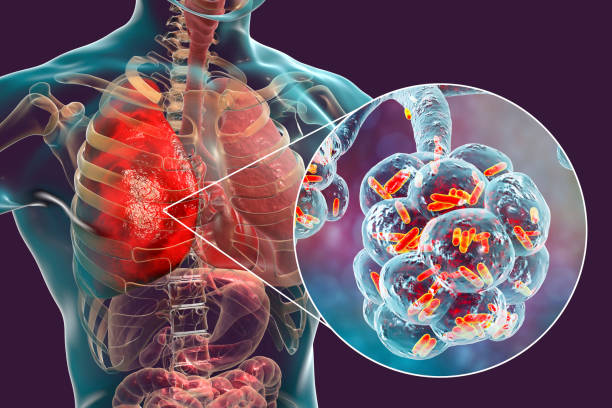
Tuberculosis (TB) is a potentially serious infectious disease that mainly affects the lungs but can also impact other parts of the body. Caused by the bacterium Mycobacterium tuberculosis, TB spreads through the air when a person with the active pulmonary disease coughs, sneezes, or even talks, releasing microscopic droplets containing the bacteria. People can get infected by inhaling these droplets. TB presents in two forms: latent, where the bacteria remain inactive in the body without causing symptoms, and active, which is symptomatic and can be contagious. If left untreated, active TB can be fatal, but with proper medical treatment, it is curable. Despite being a preventable and treatable disease, TB remains a major global health challenge, especially in areas with limited healthcare resources.
Transmission: A Breath Away
Tuberculosis is predominantly a pulmonary disease, spreading from person to person through the air. When someone with active pulmonary TB coughs, sneezes, talks, or even sings, they can release droplets containing M. tuberculosis into the air. Individuals nearby can inhale these infectious droplets, becoming exposed to the bacteria. Notably, TB is not transmitted through touch, sharing food or drink, or casual contact, which underscores the importance of airborne precautions in its prevention.
The Causative Agent: tuberculosis mycobacterium
At the heart of tuberculosis is the bacterium Mycobacterium tuberculosis (M. tuberculosis), a remarkably hardy and slow-growing microorganism. Its unique cell wall, rich in lipids, not only gives it the characteristic resistance to many common antibiotics but also enables it to evade the host’s immune defenses. This resilience is a key factor in the complexity and duration of TB treatment.
Causes of Tuberculosis
tuberculosis symptoms

Diagnosis of Tuberculosis
The diagnosis of tuberculosis (TB) involves a combination of medical history, physical examination, and several diagnostic tuberculosis tests. These tests are crucial to distinguish between latent TB infection and active tuberculosis disease, as well as to determine the location and severity of the infection. Here’s an overview of the primary methods used to diagnose TB:
1. Medical History and Physical Examination
- Symptoms Review: A healthcare provider will assess symptoms that suggest TB, such as a persistent cough, weight loss, fever, and night sweats.
- Exposure History: Information about the patient’s exposure to known TB cases, travel history to TB-endemic areas, or any history of previous TB infection or vaccination.
2. Skin Test (Mantoux tuberculosis skin test)
- Procedure: A small amount of tuberculin purified protein derivative (PPD) is injected under the skin of the forearm.
- Reading: After 48 to 72 hours, the injection site is checked for swelling or induration; a positive reaction indicates TB exposure.
3. Hematological Assessments (Interferon-Gamma Release Assays – IGRAs).
- Types: Tests like QuantiFERON-TB Gold and T-SPOT.TB measures the immune system’s response to TB bacteria.
- Advantages: IGRAs require only one patient visit, have no risk of boosting responses to subsequent tests, and are not affected by prior BCG vaccination.
4. tuberculosis chest x-ray
- Purpose: To detect abnormalities in the lungs suggestive of TB, such as cavities or infiltration.
- Limitations: While chest X-rays can suggest TB, they cannot confirm the diagnosis alone, as other diseases can cause similar abnormalities.

5. Sputum Tests
- Microscopy: Examination of sputum samples under a microscope to detect TB bacteria.
- Culture: Growing the bacteria from sputum samples to confirm the presence and identify the strain of TB; it’s the gold standard for TB diagnosis.
- Molecular Tests: Rapid tests like nucleic acid amplification tests (NAATs) can detect TB DNA or RNA in sputum samples, providing quicker results than culture.
6. CT Scans or MRIs
- Usage: These imaging tests are used for a more detailed view, especially in cases of extrapulmonary TB or when the diagnosis is uncertain.
7. Biopsy
- When Used: In cases of suspected extrapulmonary TB, a biopsy of the affected tissue can help confirm the diagnosis.
8. Drug Susceptibility Testing
- Importance: Once TB is diagnosed, it’s crucial to test the bacteria’s susceptibility to anti-tuberculosis drugs, especially to detect drug-resistant strains.
Treatment of Tuberculosis
The treatment of tuberculosis (TB) is a thorough process designed to eliminate the TB bacteria from the body, prevent the spread of the disease, and avoid the development of drug-resistant strains. Here’s a comprehensive overview of tuberculosis treatment strategies:
1. Standard Treatment Regimen
- Active TB: The typical treatment for active TB is a 6-month course of a combination of antibiotics. The most common regimen includes:
- Initial Phase (2 months): Isoniazid, rifampin, ethambutol, and pyrazinamide.
- Continuation Phase (4 months): Isoniazid and rifampin.
- Latent TB: Treatment aims to prevent the development of active TB and usually involves taking isoniazid for 6-9 months, although there are alternative regimens.
2. Monitoring and Supervision
- Directly Observed Therapy (DOT): To ensure adherence, DOT is often recommended, where a healthcare provider observes the patient taking each dose of medication.
- Regular Monitoring: Patients are regularly monitored for side effects and to ensure the effectiveness of the treatment. Liver function tests are often conducted due to the potential hepatotoxicity of some TB medications.
3. Addressing Drug-Resistant TB
- Multidrug-resistant TB (MDR-TB): Requires a longer treatment (up to 24 months) with second-line drugs that are more toxic and less effective than the standard treatment.
- Extensively drug-resistant TB (XDR-TB): Treatment is even more complex and may involve a combination of antibiotics. Potentially including newer drugs like bedaquiline and linezolid, for an extended period.
4. Supportive Care
- Nutritional Support: Adequate nutrition supports the immune system and overall health during treatment.
- Managing Side Effects: Some TB medications can have significant side effects, and managing these is crucial for the patient’s quality of life and adherence to treatment.
5. Treatment of Extrapulmonary TB
- The treatment regimen is generally similar to that for pulmonary TB, but the duration might be extended, especially for TB meningitis or bone/joint TB.
6. Patient Education
- Educating patients about the importance of adhering to the full course of treatment is vital to prevent the development of drug resistance and ensure the success of the treatment.
7. Follow-Up
- After completing treatment, patients typically undergo follow-up evaluations. Including chest X-rays and sputum tests, to ensure the infection has been fully resolved.

Prevention of Tuberculosis
Preventative measures include:
- tuberculosis vaccine: The Bacille Calmette-Guérin (BCG) vaccine can offer protection, especially in children.
- Screening and Treatment of Latent TB: Identifying and treating latent TB can prevent the progression to active TB.
- Improving Ventilation: In crowded settings, improving airflow can reduce the risk of TB transmission.
- Wearing Masks: Masks can help prevent the spread of TB in high-risk settings.
- Public Health Measures: Rapid identification and treatment of active TB, along with tracing and screening of contacts, are crucial steps in preventing the spread of TB.
The Fight Against TB: A Global Endeavor
Combating TB requires a concerted global effort, encompassing robust public health strategies, research, and collaboration. The World Health Organization’s End TB Strategy aims to dramatically reduce TB incidence. And deaths by 2030 through universal access to care, Preventive treatment for high-risk populations, and investment in TB research. Innovations in diagnostics, vaccines, and treatment are also vital to turning the tide against this persistent disease.
Conclusion
Tuberculosis is a significant global health issue, but with proper treatment and prevention strategies, it is possible to control and even eradicate this disease. Awareness, early diagnosis, and treatment adherence are crucial steps in the fight against TB. By understanding TB, individuals can take proactive steps to protect themselves. And contribute to the broader effort to eliminate this infectious disease from communities worldwide.





