Understanding Edema: Causes, Symptoms, and Treatments
Understanding Edema: Causes, Symptoms, and Treatments

Edema, commonly known as swelling, is characterized by fluid accumulation in the body’s tissues. It can affect any body part, though it’s most frequently observed in the hands, arms, feet, ankles, and legs. It can result from various causes, ranging from simple factors like prolonged standing or sitting to more complex medical conditions. This article delves into the causes, types, symptoms, diagnosis, treatment, and prevention of it, providing a thorough understanding of this common health issue.
What is Edema?
Edema results from fluid trapped in the body’s tissues, which can be due to various factors, including health conditions, lifestyle choices, and medication. It’s essential to understand that while edema itself is a sign of an underlying issue, it can also lead to complications if not addressed timely.
Causes of Edema
Various factors can contribute to the development of it, including but not limited to:
- Heart Conditions: Congestive heart failure is a common cause of edema. When the heart’s pumping efficiency is compromised, blood flow slows and can back up, leading to fluid accumulation in the tissues.
-
Renal Disease: The kidneys are essential for regulating the body’s fluid balance. Impaired kidney function can lead to fluid retention, causing edema.
- Liver Disease: Conditions like cirrhosis can impair liver function, affecting fluid regulation and leading to fluid accumulation, especially in the abdominal cavity (ascites).
- Venous Insufficiency: Damage or dysfunction in the vein valves, especially in the legs, can cause blood to pool and increase pressure within the veins, leading to fluid leakage into surrounding tissues.
- Lymphatic System Disorders: When the lymphatic system is compromised, it cannot effectively remove excess fluid from tissues, resulting in edema.
- Inflammation: Inflammatory processes can increase the permeability of blood vessels, allowing more fluid to escape into the surrounding tissues, which can lead to swelling.
- Medications: Certain drugs, including blood pressure medications, steroids, and nonsteroidal anti-inflammatory drugs (NSAIDs), can cause or worsen edema.
- Pregnancy: Hormonal changes during pregnancy can lead to increased fluid retention, contributing to edema. Additionally, the growing uterus can exert pressure on veins in the pelvis, impairing blood flow from the legs and leading to swelling.
- Dietary Factors: Excessive salt intake can lead to fluid retention, contributing to edema.
- Sedentary Lifestyle: Lack of physical activity can impede blood flow, especially in the legs, leading to fluid accumulation.
- Infections or Injuries: Infections, burns, and traumatic injuries can lead to localized edema as part of the inflammatory response.
Symptoms of Edema
The symptoms of edema depend on its location and severity. Common signs include:
-
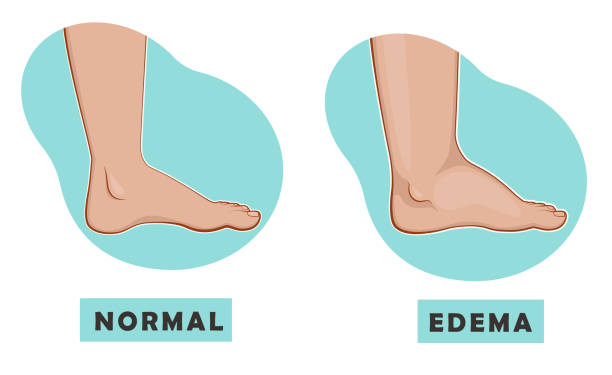
Swelling or Puffiness:
One of the most noticeable signs of edema is the swelling or puffiness of the skin, which can occur in specific areas (localized edema) or throughout the body (generalized edema).
-
Stretched or Shiny Skin:
The skin over the affected area may appear stretched, shiny, or glossy due to the increased fluid pressure underneath.

-
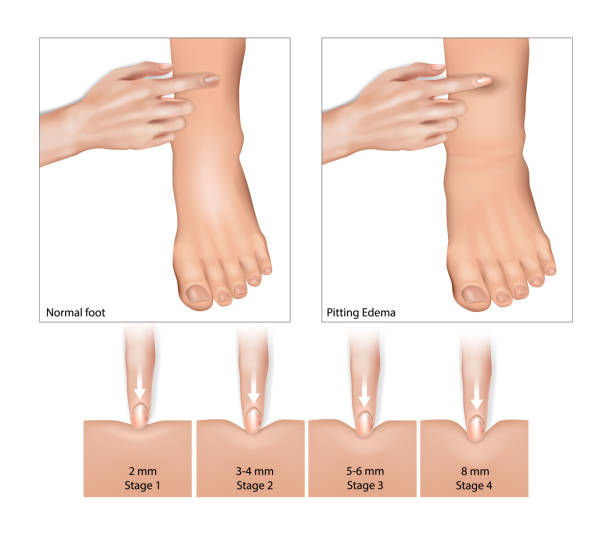
Skin that Retains a Dimple (Pitting Edema):
When you press on the swollen skin for a few seconds and then release, an indentation or dimple may remain. This is known as pitting edema.
-
Non-pitting Edema:
In some cases, when the skin is pressed, it does not leave a dimple. This is referred to as non-pitting edema and can be indicative of certain types of edema, such as lymphedema.
-
Increased Abdominal Size:
In cases of abdominal edema, or ascites, there can be a noticeable increase in the size of the abdomen.
-
Stiffness or Limited Movement:
Swelling in joints or limbs can lead to a range of motion limitations, stiffness, or discomfort in the affected areas.
-
Pain or Aching:
The affected area might feel painful or achy, especially if the edema is due to inflammation or injury.
-
Increased Weight:
Generalized edema can lead to a sudden increase in body weight due to the accumulation of excess fluid.
-
Changes in Urination:
In cases where edema is related to kidney or heart issues, changes in urination patterns, such as increased night-time urination or foamy urine, might be observed.
-
Shortness of Breath:
If edema is related to heart disease or pulmonary edema, shortness of breath might occur, especially when lying down or during physical exertion.
-
Elevated Blood Pressure:
In some instances, edema can be associated with increased blood pressure, particularly when related to kidney or cardiovascular conditions.
Recognizing these symptoms early can aid in timely diagnosis and treatment, addressing the underlying cause and mitigating the effects of edema. If you experience unexplained or persistent swelling, it’s crucial to consult a healthcare provider for a thorough evaluation.
Diagnosis
To diagnose it, healthcare providers will review medical history, perform a physical examination, and may order tests such as blood tests, urine analyses, or imaging studies to identify the underlying cause.
Treatment and Management
Treatment and management of focus on addressing the underlying cause, reducing swelling, and preventing complications. Here’s an overview of the common strategies used to treat and manage edema:
-
Addressing the Underlying Cause:
Identifying and treating the root cause of edema is crucial. This may involve managing heart failure, kidney disease, liver problems, or addressing any other specific conditions contributing to fluid retention.
-
Lifestyle Modifications:
- Dietary Changes: Reducing salt intake can help decrease fluid retention. Patients are frequently recommended to adhere to a diet low in sodium.
- Fluid Intake: Depending on the underlying cause, adjusting fluid intake might be necessary.
- Exercise: Regular physical activity, especially activities like walking or swimming, can improve circulation and help reduce fluid buildup, particularly in the legs.
- Weight Management: Achieving and maintaining a healthy weight can reduce the risk of developing edema and alleviate symptoms.
-
Medications:
-
- Diuretics: Often referred to as water pills, diuretics help the body eliminate excess fluid through urination. They are commonly prescribed for edema, but the type and dosage depend on the underlying condition and individual patient needs.
- Adjusting Current Medications: If a medication is contributing to edema, a healthcare provider may adjust the dosage or switch to an alternative treatment.
-
Compression Therapy:
For edema in the limbs, wearing compression stockings, sleeves, or bandages can help maintain pressure on the tissues, preventing fluid from accumulating.
-
Elevation:
Elevating the affected body part above the level of the heart, especially for leg edema, can help reduce swelling and encourage fluid drainage.
-
Physical Therapy:
Physical therapists can provide exercises and manual therapies to improve fluid movement and reduce swelling, particularly in cases of lymphedema.
-
Massage:
A gentle massage or specialized manual lymph drainage techniques can help move fluid out of the affected area.
Proper skin care is important to prevent skin breakdown and infections, especially in areas affected by it.
-
Monitoring:
Regular monitoring of weight and edema symptoms can help assess the effectiveness of treatment and detect any worsening of the condition.
-
Avoiding Prolonged Sitting or Standing:
Regular movement or changing positions can help prevent fluid from pooling, especially in the legs.
Individuals with it need to work closely with their healthcare provider to develop a treatment plan tailored to their specific needs and underlying conditions. Regular follow-ups and adjustments to the treatment plan may be necessary based on the individual’s response to therapy.

Preventing Edema
Preventing edema involves a combination of lifestyle adjustments and medical interventions, especially if you’re predisposed to conditions that cause swelling. Here are some strategies to help prevent edema:
- Reduce Salt Intake: Excessive salt in the diet can cause the body to retain water, leading to swelling. Aim to limit your salt intake by avoiding processed foods, seasoning your meals with herbs and spices instead of salt, and choosing low-sodium versions of products.
- Maintain a Healthy Weight: Being overweight can increase the pressure on your veins, contributing to fluid accumulation.
- Exercise Regularly: Physical activity helps stimulate circulation and can prevent fluid from accumulating, especially in the legs. Even simple activities like walking, swimming, or cycling can be beneficial.
- Elevate Your Legs: When sitting or lying down for extended periods, elevate your legs above your heart level to improve circulation and prevent fluid buildup.
- Avoid Prolonged Standing or Sitting: Change your position frequently and take breaks to move around if you need to stand or sit for a long time.
- Wear Compression Garments: Compression stockings or sleeves can help prevent fluid from accumulating in the limbs, particularly if you’re prone to edema or have a job that requires prolonged standing or sitting.
- Stay Hydrated: Oddly enough, staying hydrated can help prevent fluid retention. When your body is dehydrated, it tends to hold onto fluid, so ensuring adequate fluid intake can help reduce swelling.
- Manage Chronic Conditions: If you have conditions like heart failure, kidney disease, or liver disease, managing these conditions effectively is crucial to preventing edema.
- Monitor Medication Side Effects: Some medications can cause or worsen edema. If you notice swelling after starting a new medication, consult your healthcare provider. They may adjust your dosage or change medications.
- Regular Medical Check-Ups: Regular visits to your healthcare provider can help detect potential issues early before they lead to edema.
When to Seek Medical Attention
It’s essential to consult a healthcare provider if you experience unexplained swelling, especially if it’s accompanied by other symptoms like difficulty breathing, chest pain, or confusion. These could indicate a serious underlying condition requiring immediate attention.
Conclusion
It is a condition that manifests through visible swelling, caused by fluid accumulation in the body’s tissues. While it can sometimes be a benign symptom of a minor issue, it can also signal more serious health problems. Understanding the underlying causes, recognizing the symptoms, and seeking appropriate medical care are vital steps in managing edema effectively. Through a combination of lifestyle changes and medical treatment, individuals can manage their symptoms and improve their quality of life.





